Why Our Baby? Pre-Natal Diagnosis
Why Our Baby? Pre-Natal Diagnosis
PRENATAL DIAGNOSIS
All women, in Ireland, have access to ultrasound services, which can assess their baby for problems or anomalies. Around 2-3% of pregnancies do have some congenital anomalies and of this a small number are life-limiting, meaning that there is a condition present affecting the fetus that is likely to lead to early pregnancy loss either before birth, around the time of birth or death in infancy.
The initial effect of hearing during pregnancy that your baby is not the healthy baby you anticipated is traumatic. During the days, weeks and, indeed, months that follow, there will be many additional concerns. You may worry about what the baby will look like, about the baby dying in the womb or at birth, or about the labour starting early. There will be concerns about the actual birth, about the baby actually surviving and the responsibility of caring for a baby with problems. There can be a feeling of helplessness and of a lack of control of your life. You may doubt the diagnosis and try to convince yourself that it is all a mistake. It is hard to accept that your baby may not live.
The following extract is from PATHWAY FOR MANAGEMENT OF FATAL FETAL ANOMALIES AND/OR LIFE-LIMITING CONDITIONS DIAGNOSED DURING PREGNANCY – PERINATAL PALLIATIVE CARE by Professor Keelin O Donoghue, National Implementation Group, HSE Standards for Bereavement Care following Pregnancy Loss and Perinatal Death, January 2019
https://pregnancyandinfantloss.ie/perinatal-palliative-care-pathway/
“ Structural anomalies are suspected or diagnosed at routine ultrasound screening in the first or second trimester of pregnancy. They can also be seen at routine scans carried out as part of general antenatal care at any stage including late pregnancy. It is important to note that ultrasound scans will not identify all structural anomalies.
The Obstetrician or the Midwife/Sonographer performing a routine booking/dating or anomaly ultrasound scan may be faced with the initial breaking of bad news to the pregnant woman and partner. A second opinion may be sought in such circumstances. Those performing the initial scan should respond to Parents’ questions with whatever information is available at the time.
Prompt referral to a fetal medicine specialist ideally within 24 to 72 hours is the standard of care where a major fetal anomaly is suspected followed by provision of written information resources and support. While awaiting referral the Parents should be given contact details of a support person in the referring hospital.
Some fetal conditions for which there are simple definitive diagnostic tests and an unequivocal prognosis (e.g.T13, T18, anencephaly), may be diagnosed and managed entirely at local hospital level, especially where fetal medicine expertise exists. In other cases, invasive testing may occur at the tertiary unit, but the results are communicated to local units and ongoing care is managed with the local obstetricians and neonatologists/paediatricians, supported as needed by the tertiary site.
A fetal medicine specialist is a medical practitioner who is actively practicing in the area of fetal medicine. The fetal medical specialist has undergone specific further training either through an approved Maternal-Fetal Medicine (MFM) fellowship or a higher qualification in diagnostic ultrasound or has a long-term expertise in ultrasound/fetal medicine and trained at a time before these fellowships/qualifications were available.
A fetal medicine specialist should confirm the antenatal diagnosis of a structural anomaly and a suspected fatal fetal anomaly/life limiting condition (FFA/LLC). This will usually involve performing diagnostic ultrasound on an appropriate, functioning, up to date ultrasound machine. Further invasive investigations including amniocentesis, chorionic villus sampling, fetal blood sampling to establish the fetal genetic profile, in addition to maternal bloods and fetal MRI to confirm the diagnosis or to add further information may be necessary.
These investigations should be followed by a multidisciplinary team discussion to agree the diagnosis and prognosis and to consider any implications for maternal health and antenatal care. The diagnosis and prognosis is then explained and discussed with the Parents.
A perinatal palliative care approach is appropriate for parents who continue their pregnancy after antenatal diagnosis of fatal fetal anomalies, as well as for those who opt for termination of pregnancy, in accordance with the Health (Regulation of Termination of Pregnancy) Act 2018.”
Families who receive the diagnosis of fatal fetal anomaly/life limiting condition, which cannot be corrected at birth, will receive clear, accurate and concise information, support and counselling to help them with their decision-making. If your baby with trisomy also has an immediate life-threatening diagnosis e.g. a serious heart defect you and your doctors will discuss the considerations and risks involved in treatments. A perinatal palliative care approach is appropriate for parents who continue their pregnancy after antenatal diagnosis of fatal fetal anomalies, as well as for those who opt for termination of pregnancy. Each baby with trisomy is unique and what is right for one baby is not necessarily right for another.
Maternal health and wellbeing during pregnancy, birth and postnatal period remain the clear focus of care. Bereavement support and accompaniment is provided by the clinical nurse/midwife specialist all along the care pathway and continuing through the baby’s life span and beyond.
The initial effect of hearing that your baby is not the healthy baby you expected is very traumatic. A “family-centred” perspective is needed to gain much valued support from those in your nearest network and also, to allow your family to be involved in the shortened life of your baby. Your team will support you in sharing the diagnosis with siblings and extended family. An important aspect of coping with this heart-breaking situation is that you treasure every moment with your baby. This is called “continued bond” and it’s about remembering that you continue to be parents to this baby, despite the diagnosis and despite the shortened lifetime. You will be encouraged to think about a “birth-plan”, the things that are important to you for when your baby is delivered, whether your baby is living at delivery or whether he/ she has died before delivery. Even if your baby’s lifetime is limited to a few months in the womb, or a matter of hours, days or months in this world, her life can be a positive experience
Support organisations like S.O.F.T. Ireland put parents in contact with other parents who have gone through a similar experience and feedback indicates this has been very beneficial.
PRE-NATAL DIAGNOSTIC TEST
Non-invasive prenatal testing (NIPT)
NIPT is a blood test taken from a pregnant woman to assess the chance of the baby having trisomy 21, trisomy 18 or trisomy 13. This is a screening test, not a diagnostic test, and has limitations.
Further information is available at:
Chorionic Villus Sampling (CVS)
This is an invasive diagnostic test. CVS is usually performed between 11+0 weeks and 13+6 weeks of gestation. This is a procedure where a sample of the placenta tissue is obtained for testing.
Amniocentesis
This is an invasive diagnostic test. Amniocentesis is usually offered from 15+0 weeks’ gestation. This is a procedure where a sample of amniotic fluid is obtained for testing for similar disorders as CVS
Further information on CVS and amniocentesis is available at :-
https://www.rcog.org.uk/en/guidelines-research-services/guidelines/gtg8/
Pathway for Management of Fatal Fetal Anomalies/Life Limiting Conditions Diagnosed during Pregnancy
(Dr. Keelin ODonoghue 2019)
Baby has a fatal fetal anomaly / life-limiting or potentially life-limiting condition confirmed antenatally
Discuss at formal fetal medicine MDT meeting and determine care options
Offer consultation with other professionals e.g neonatology, genetics, paediatrics
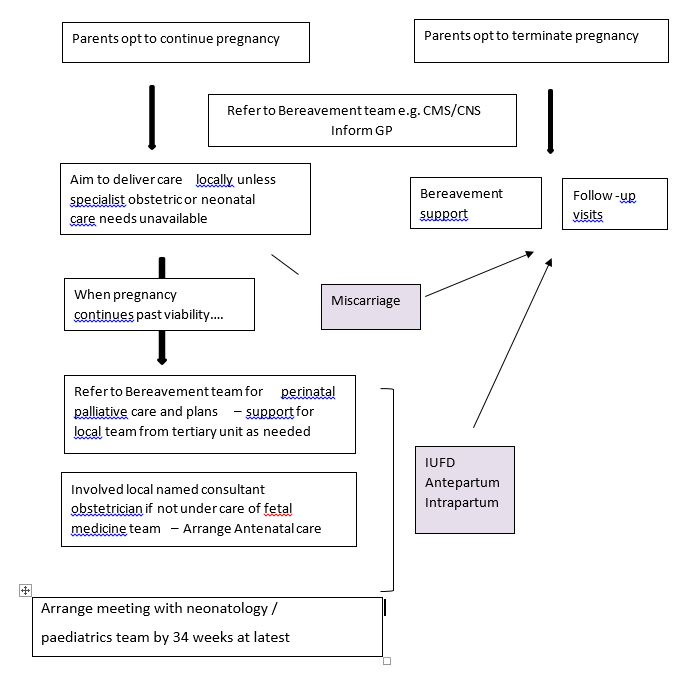
MDT discussion and agreement between members of team – regarding timing and mode of delivery – personnel to be involved – parents’ birth plans. Detailed care plan to be in notes. Plans for term and preterm delivery as well as parallel planning where neonatal survival.
Talking to support groups like S.O.F.T. Ireland in the antenatal period is very important as they are made up of mothers and fathers who have experienced a similar and equally devastating diagnosis as you have.
See S.O.F.T. Ireland Trisomy 13/18 Pre-Natal Diagnosis Support and Information Leaflet which is available in all maternity hospitals.
Pregnancy and Infant Loss Ireland
https://pregnancyandinfantloss.ie/
Unique – Rare Chromosome Disorder Support Group
